News Release
Good Vibrations: Using Light-Heated Water to Deliver Drugs
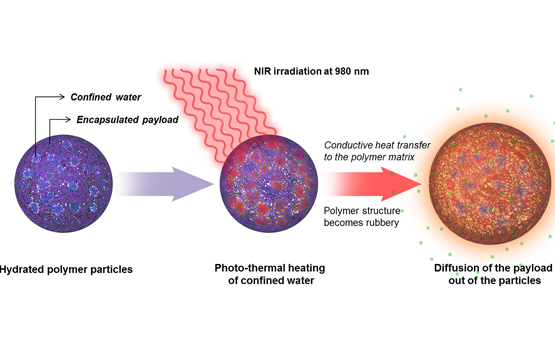 |
| In this schematic representation, a hydrated polymeric nanoparticle is exposed to near-infrared light. The NIR heats pockets of water inside the nanoparticle, causing the polymer soften and allowing encapsulated molecules to diffuse into the surrounding environment. |
Researchers use near-infrared light to warm water-infused polymeric particles
San Diego, Calif., April 4, 2014 -- In this schematic representation, a hydrated polymeric nanoparticle is exposed to near-infrared light. The NIR heats pockets of water inside the nanoparticle, causing the polymer soften and allowing encapsulated molecules to diffuse into the surrounding environment.
Researchers from the University of California, San Diego Skaggs School of Pharmacy and Pharmaceutical Sciences, in collaboration with materials scientists, engineers and neurobiologists, have discovered a new mechanism for using light to activate drug-delivering nanoparticles and other targeted therapeutic substances inside the body.
This discovery represents a major innovation, said Adah Almutairi, PhD, associate professor and director of the joint Â鶹´«Ã½-KACST Center of Excellence in Nanomedicine. Up to now, she said, only a handful of strategies using light-triggered release from nanoparticles have been reported.
The mechanism, described in the April 1, 2014 online issue of ACS Nano, employs near-infrared (NIR) light from a low-power laser to heat pockets of water trapped within non-photo-responsive polymeric nanoparticles infused with drugs. The water pockets absorb the light energy as heat, which softens the encapsulating polymer and allows the drug to be released into the surrounding tissue. The process can be repeated multiple times, with precise control of the amount and dispersal of the drug.
“A key advantage of this mechanism is that it should be compatible with almost any polymer, even those that are commercially available,” said Mathieu Viger, a post-doctoral fellow in Almutairi’s laboratory and co-lead author of the study. “We’ve observed trapping of water within particles composed of all the biodegradable polymers we’ve so far tested.”
The method, noted Viger, could thus be easily adopted by many biological laboratories.
The combined use of hydrated polymers and near-infrared light appears to resolve a host of technological and health barriers that have hindered previous, similar approaches. Earlier efforts to use NIR-triggered release have not been widely exploited because they required special designer polymers, expensive high-powered lasers and/or the co-encapsulation of inorganic particles whose safety in the body remains questionable.
The new method described by Almutairi and colleagues in the departments of Mechanical and Aerospace Engineering, Neuroscience, and Chemistry and Biochemistry at Â鶹´«Ã½ uses NIR at a vibrational wavelength cued to excite water molecules, which absorb the optical energy and convert it to heat. NIR is capable of penetrating biological tissues to greater depths than visible or ultraviolet light. Almutairi is affliated with the Department of NanoEngineering at Â鶹´«Ã½ Jacobs School of Engineering.
Co-lead author Wangzhong Sheng, a graduate student in Department of Mechanical and Aerospace Engineering, explained the selectivity of heating by comparing the trapped water within particles to a glass of water and the surrounding water within the solution or tissue to a bathtub. The smaller amount of water is heated much more rapidly because of the enormous volume difference.
An obvious use of the method, said Almutairi, is light-triggered drug delivery, but with more research, she anticipates the new method could provide a variety of industrial, medical and scientific applications, including “any technological application requiring that chemistry be controlled in time and in space, such as in catalysis or self-repairing materials or light-activated sunscreens or pesticide dosing.”
Co-authors include Carl-Johan Carling, Jacques Lux and Caroline de Gracia Lux, UCSD Skaggs School of Pharmacy and Pharmaceutical Sciences; Kim Dore and Roberto Malinow, UCSD Department of Neurosciences; Ali H. Alhasan, UCSD Skaggs School of Pharmacy and Pharmaceutical Sciences and UCSD Center of Excellence in Nanomedicine; and Madeleine Grossman, UCSD Department of Chemistry and Biochemistry.
Funding for this research came, in part, from a National Institutes of Health New Innovator Award (1 DP2 OD006499-01) and NIH grant R01AG032132. This research is in partnership with the King Abdulaziz City of Science and Technology.
Media Contacts
Scott LaFee
UCSD Health Sciences
619-543-6163
slafee@ucsd.edu